Glaucoma
WHAT IS GLAUCOMA?
Building up Pressure

Causes Optic Nerve
Open-angle glaucoma occurs when the eye’s drainage system becomes clogged overtime
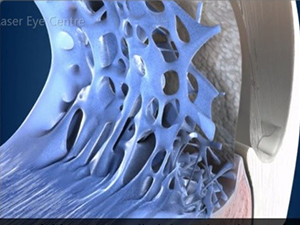
A part of this system, called the trabecular mechwork
Who is at risk of Glaucoma?
Everyone is at risk of Glaucoma. However certain groups are at higher risk than others. The following groups are at a higher risk of developing Glaucoma:
- Africans (six to eight times more common than in Caucasians)
- People over 60 years of age
- Family members with glaucoma (risk factor increases by four to nine times)
- Asians (primary angle closure glaucoma)
- Steroid users
- Those who have had eye injuries
- Diabetics
- Previously done eye operation like Cataract, corneal transplant can lead to glaucoma
Types of glaucoma:
- Primary open angle glaucoma(Chronic simple Glaucoma)
- Primary closed angle glaucoma.
- Secondary open angle glaucoma.
- Low tension Glaucoma.
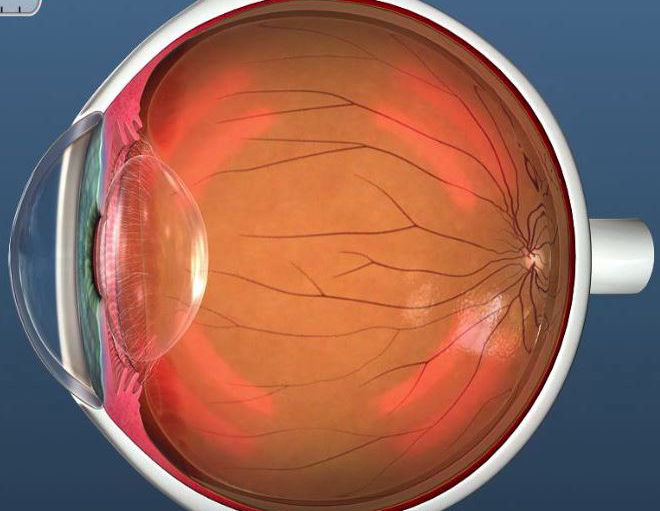
- Primary open angle glaucoma (also known as Chronic Simple Glaucoma) – (POAG) is the most common type of glaucoma. Formation of the fluid in the eye gives nutrition to the crystal lenses of the cornea, after giving nutrition to the eye fluid is drained in the anterior chamber. In any given time, there is proper balance in the drainage of the fluid, when the balance is broken it can damage the delicate part of the eye including optic nerve.


DIAGNOSIS FOR GLAUCOMA
1. CHECKING INTRA-OCULAR PRESSURE
Intra-Ocular pressure is checked by a Tonometer which is known
as Applanation tonometry around 3 millimeter of the Applanation tonometer, normal pressure is about 16-17mm of mercury. Here cornea is indented and pressure of the eye is recorded. Here thickness’ of the cornea is an important factor.


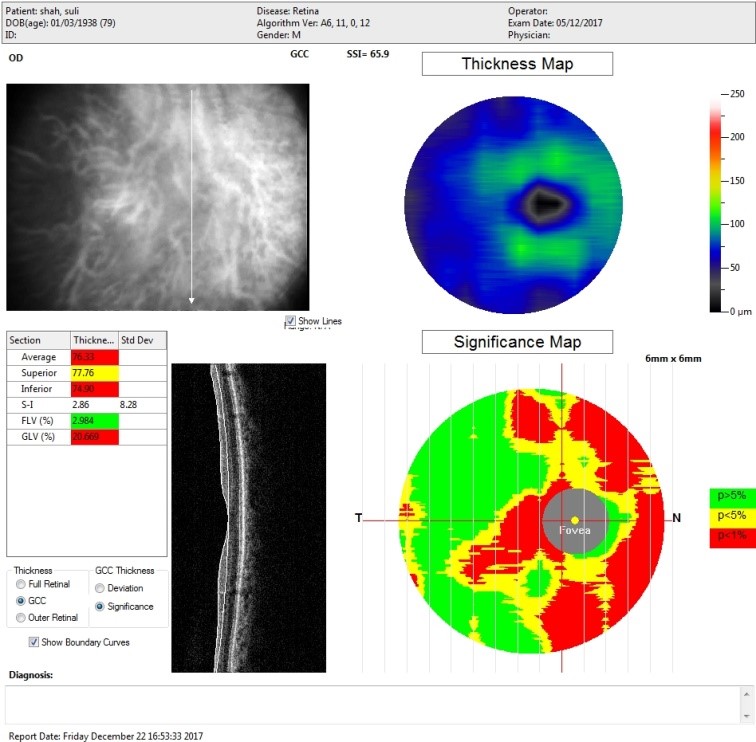
2. OPTICAL COHERENCE TOMOGRAPHY TEST (OCT)

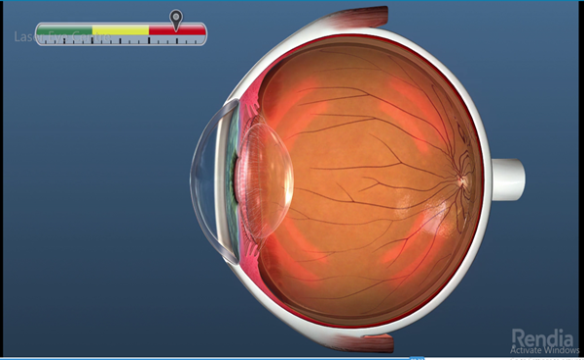
In glaucoma the cup of the optic nerve starts enlarging and becoming deep and there is a shifting of the cup on the nasal side and blood vessels are going on the other side. Because of the high pressure going from the optic nerve, center of the retina is damaged.
Diagnosis of Glaucoma can be established by structural changes due to intraocular pressure on OCT examination or functional changes due to high intraocular pressure damaging the optic nerve.
What is optic nerve? It is a paired nerve that transmits visual information from the retina to the brain.
Optical coherence tomography (OCT) is a commonly used imaging modality in the evaluation of glaucoma. This machine will detect how much damage glaucoma has done to the optic nerve and central part of retina.
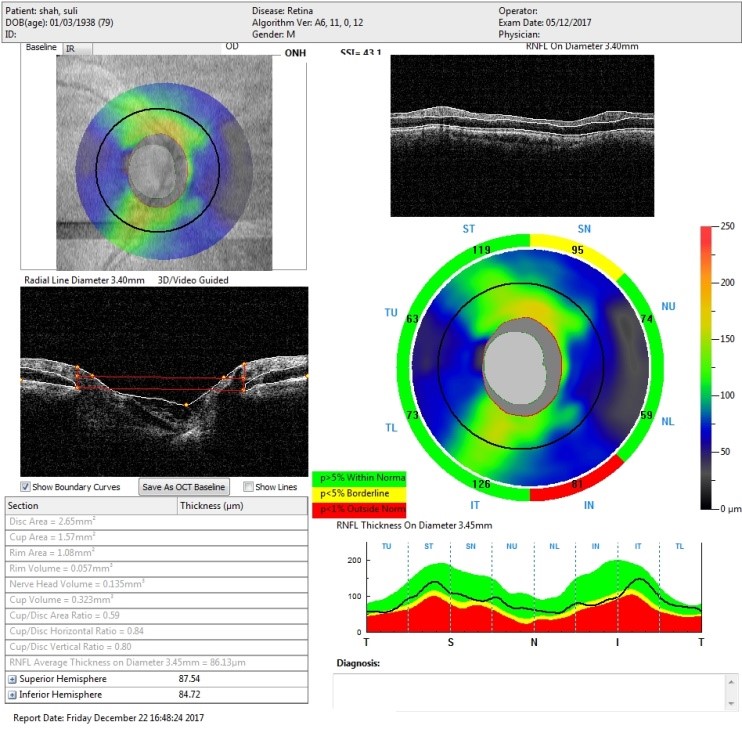
Optic Nerve Normal head here the white area
Cup of the Optic Nerve is enlarging ( white area)
3. DIAGNOSIS(FIELD ANALYTICS)

Due to high pressure inside the eye it damages the optic nerve and its fibres. This creates damage in the visual fields. It is an important tool in the diagnosis and management of Glaucoma.
It is used to examine the patient’s visual field, at least three times in a year to evaluate the severity and to monitor progression of the disease.
HOW IT IS DONE
As shown in the diagram in dark room the patient is asked to look at the black screen of Field Analyzer and technician is going to show blinking lights coming from side to the center and patient is given hand held beeper to alert technician when patient sees the light. At the end of examination visual field is displayed on the chart as shown below.
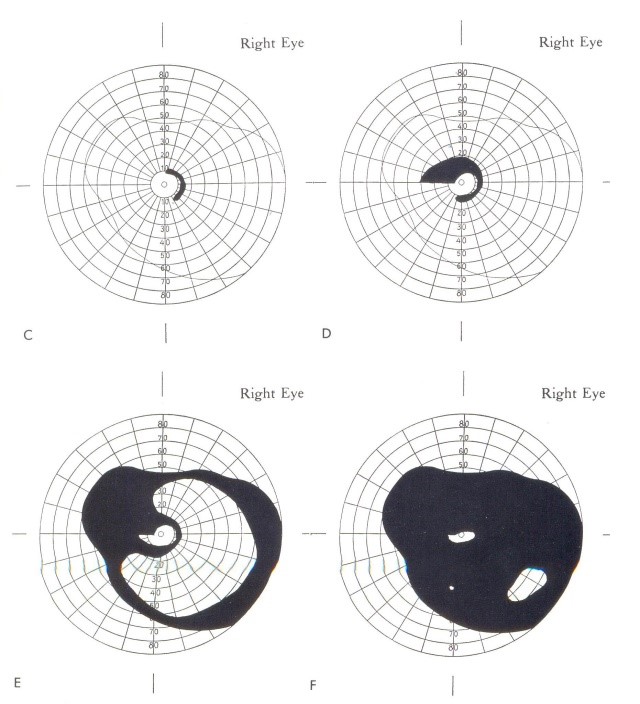
Key to Key read above diagram Top Left no. 1: area in black is showing early field defect.
Top Right No. 2: is showing moderate field defect.
Bottom Left No. 3: Advance Field defect
Bottom Right No 4: is showing very advanced field defect almost leading to blindness

Normal field defect

Field defect in Glaucoma
TREATMENT OPTIONS
Treatment for glaucoma aims to lower the internal pressure of the eye and prevent any loss of vision, or any further deterioration in the vision. Options include medicine given as eye drops, laser treatment and surgery. Regrettably, treatment cannot reverse any existing optic nerve damage, but it aims to stop further damage
- Medical line of the treatment
- Glaucoma operation
- The Laser Trabeculoplasty
MEDICAL LINE OF TREATMENT
There are several different types of medicines available for treating glaucoma; they help lower the internal pressure of the eye by increasing the flow of the fluid out, through the trabecular meshwork, or by reducing the production of fluid. The various classes of medication include:
- Beta-blockers: such as Timolol are the second most often used class of medication and work by decreasing production of fluid. Timolol is also available in a preservative-free formulation. Beta-blockers lower the pressure inside the eye by reducing how much fluid (aqueous humor) is produced in the eye. Reducing pressure in the eyes helps slow optic nerve damage, decreasing the rate of vision loss.
- Prostaglandins: include Xalatan® (latanoprost), Lumigan® (bimatoprost), Travatan Z® (Travoprost), and Zioptan™ (tafluprost), and they work by increasing the outflow of fluid from the eye. Prostaglandin analogs work by increasing the outflow of intraocular fluid from the eye. … They are effective at reducing intraocular pressure in people who have open-angle glaucoma.
- Alpha agonists [Alphagan®P (brimonidine), Iopidine®] work to both decrease production of fluid and increase drainage. Alphagan P has a purite preservative that breaks down into natural tear components and may be better tolerated in people who have allergic reactions to preservatives in other eye drops. They work by decreasing the production of aqueous fluid by the ciliary bodies of the eye and also by increasing uveoscleral outflow.
- Carbonic anhydrase inhibitors (CAIs) reduce eye pressure by decreasing the production of intraocular fluid. These are available as eye drops [Trusopt® (dorzolamide), Azopt® (brinzolamide)] as well as pills [Diamox (acetazolamide) and Neptazane® (methazolamide)].
What if eye drops do not work?
In some patients inspite of using above combination of eye drops pressure of the eye is not controlled and is likely to damage the optic nerve, in such cases Glaucoma operation is recommended. Patients coming from remote area or patients who are not likely to put the glaucoma eye drops are suggested to have surgery.
1. SURGERY
Who requires the surgery for Glaucoma?
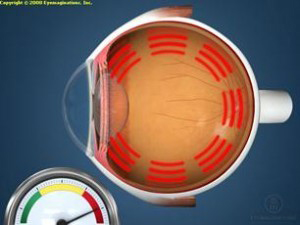
A patient who in spite of being put on medical line of treatment is unable control the intraocular pressure or when the damage to the eye sight continues, then a procedure known as trabeculectomy will be done on the patient, around 90% of these procedures have been successful.
2. TRABECULECTOMY PROCEDURE
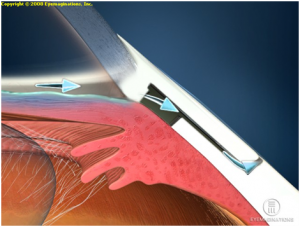
i). During a trabeculectomy, an alternative channel is created through which the fluid inside of the eye can exit when the usual pathways become blocked.
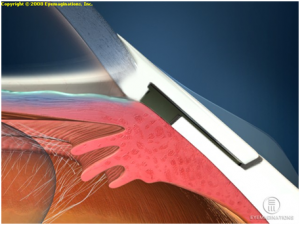
ii). The fluid is collected outside of the eye in a tiny pocket where it is then reabsorbed by the body.
High Pressure before the surgery
Pressure reduced after surgery
iii). The treatments are intended to relieve the pressure of the eye and prevent further damage to the optic nerve
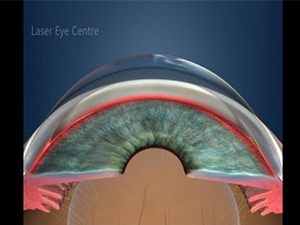
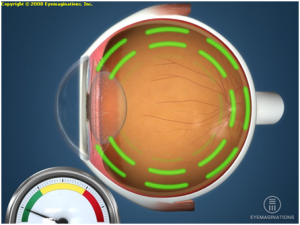
3. LASER TREATMENT
Laser can be used to open the holes in the trabecular meshwork. The procedure is usually quick and causes little discomfort. The success of this type of treatment varies from a person to person and it may be necessary to continue the eye drops after the laser treatment, though it is often prescribed at a lower dose.
Laser treatment for Glaucoma is done when eye drops fail and Glaucoma operation cannot be done.
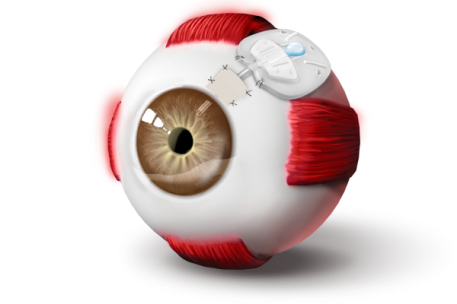
4. AHMED VALVE
Some cases of glaucoma are complicated and in failed trabeculectomy operation ( 2%-5%) another option is to put a special valve in the eye as shown in the below figure to reduce the pressure.